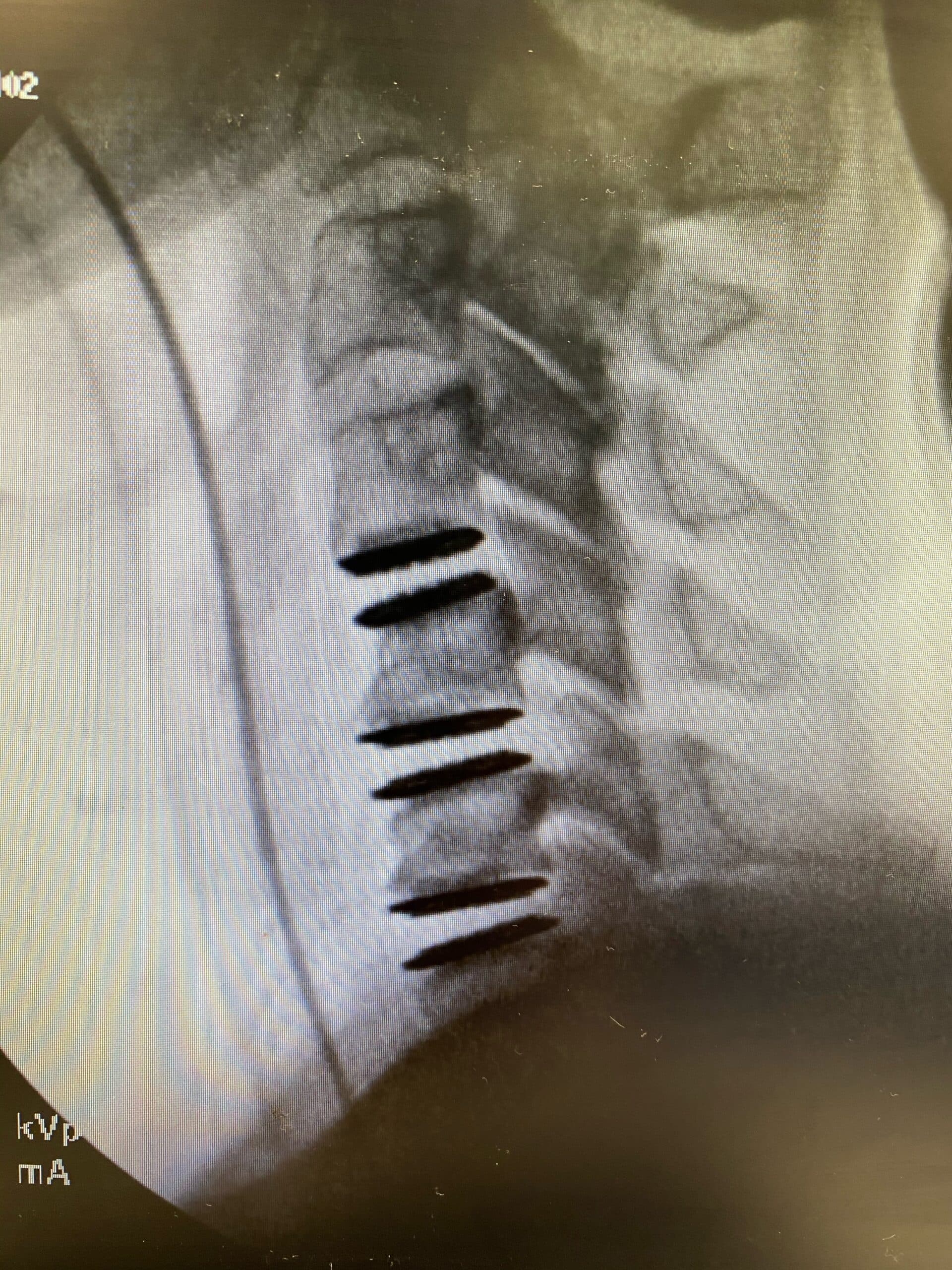
Dr. Schuler Performs Region’s First Three-Level Cervical Disc Replacement
BREAKING NEWS–December 2, 2020, Reston, Virginia — Dr. Thomas Schuler performed the first three-level artificial cervical disc replacement in the mid-Atlantic region. His patient had suffered from significant neck pain with headaches for 3 years prior to surgery. The symptoms started to include her arms, with radiating pain, numbness, and tingling. She failed to make lasting improvements with diligent physical therapy, medications, rest, time, and activity modification. She was diagnosed with significant disc degeneration at C4/5, C5/6, and C6/7 (the 3 most common levels to degenerate and become problematic). Dr. Schuler was hopeful to perform an arthroplasty at all three levels, but counseled the patient on the possibility of a hybrid construct, which is a combination of fusion and arthroplasty implants. During surgery, he was able to replace all three levels with the M6, motion-preserving implant. She tolerated the surgery well, was discharged from the hospital the following day, and is home recovering as expected.
What is a three-level disc replacement, or ACDR?
3-level cervical disc replacement is a surgical procedure aimed at providing long-term pain relief and improved mobility for patients with degenerative disc disease in the neck. While less common than 2-level disc replacement, when performed by skilled surgeons, this procedure can offer significant benefits with a reduced need for revision surgeries. By replacing the damaged discs at three adjacent levels in the cervical spine, this technique aims to alleviate pain, restore stability, and promote a healthier neck function.
A disc replacement procedure is similar to a fusion procedure in that the damaged disc is removed in its entirety and something is put in its place. The ‘something’ is where these two surgeries differ. In a fusion surgery, the empty space is filled with a stabilizer, usually a combination of a cage filled with a bone graft which either screws into the bones above and below or a plate is screwed into the bones to hold everything in place as it heals. The specific items used to stabilize the spine can vary, but the purpose is the same, which is to allow the bone graft to grow and connect to the bones above and below the disc space. The goal is for that segment to become one solid piece of bone that does not move.
With a disc replacement procedure, the empty space is not actually filled with a new disc that is made of cartilage and ligament like the native disc. Instead, the empty space is filled with a motion-preserving implant. These implants are a similar concept to a hip or knee replacement, in that they allow for motion to be maintained. The goal of a disc replacement or arthroplasty procedure is to allow for the restoration of a more natural type of motion.
The benefits of restoring motion include improving the function of the patient through movement, less downtime after surgery, and transferring less additional stress to the remaining discs in the spine. Disc replacements can be done both in the cervical spine (ACDR) and lumbar spine (LDR).
There are a number of considerations your spine surgeon will review when contemplating an ACDR. Some of these include:
- What is the degree of disc degeneration and how does that impact the patient’s motion? If the segment is not moving preoperatively, a motion-preserving implant may not be worthwhile if there is no motion to preserve.
- What is the alignment of the spine? Some alignment pathologies are best fixed with a fusion procedure to restore a more natural alignment and proper balance.
- Has there been a surgery at or near the disc level of pathology and how might that affect the new implant?
- Is there severe stenosis? How much pressure must be taken off of the neural elements and does this impact the structures surrounding the implant needed for stabilization?
After an ACDR, patients often stay just one night in the hospital for observation. They go home from the hospital with a foam collar just for comfort but is not required for healing. Patients are instructed to take it easy and avoid aggressive activities for about 6 weeks but can begin working from home as soon as the effects of the anesthesia have worn off. Feeling comfortable driving to work and completing a full day at a desk job often occurs after 2 weeks. Walking is encouraged immediately following surgery. The timing of increasing to a more vigorous fitness routine is based on the patient’s individual recovery and the number of levels replaced. Once recovered, the goal is for the patient to return to their desired lifestyle, however, smart choices are encouraged to avoid future injuries. If you are suffering from chronic neck or back pain, schedule a consultation with a spine specialist.
Topics covered
About the Author
Featured Resources
Insights to Achieve a Pain-Free Life