Spine Surgery
The future of spine surgery is now.
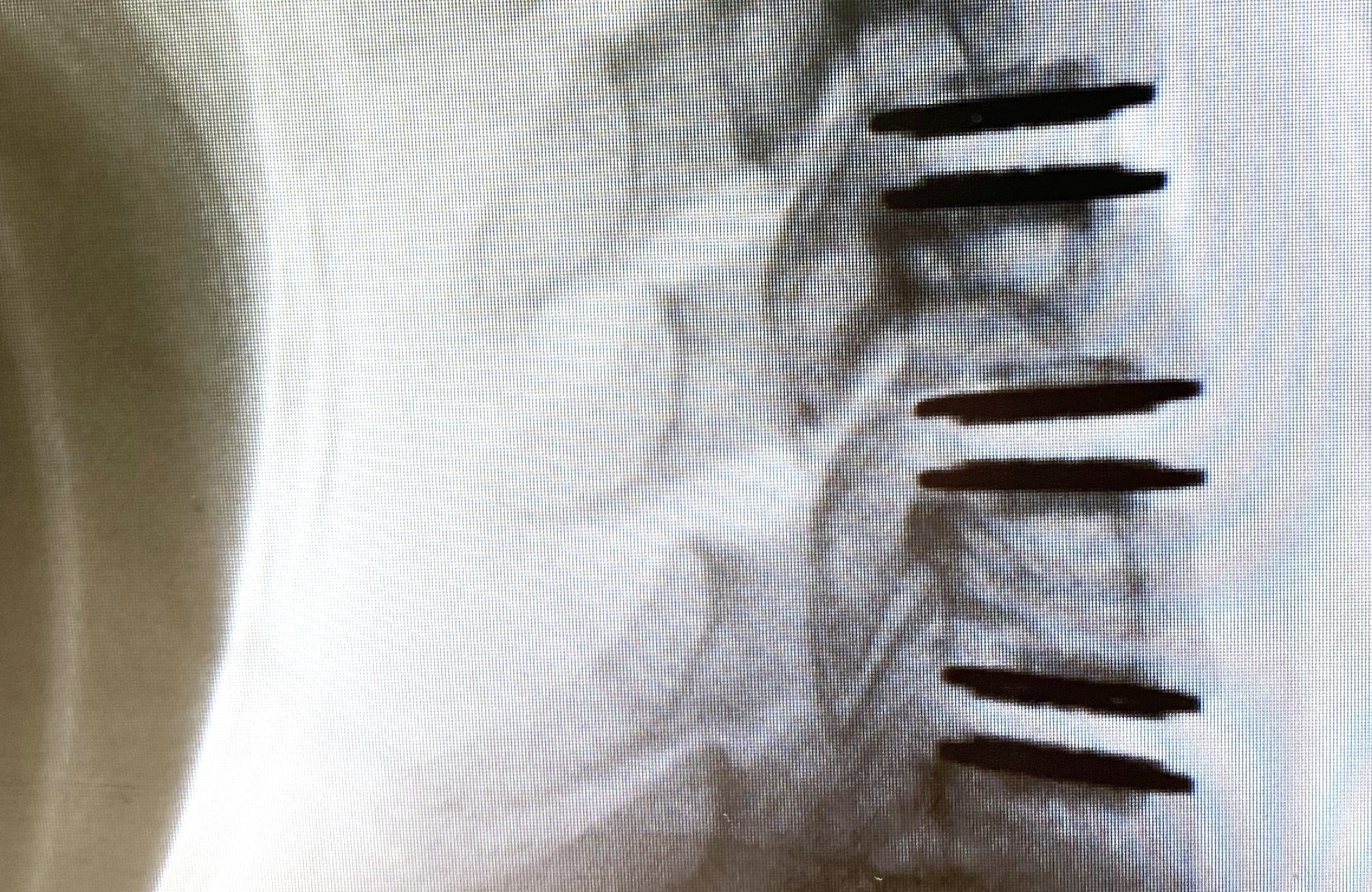
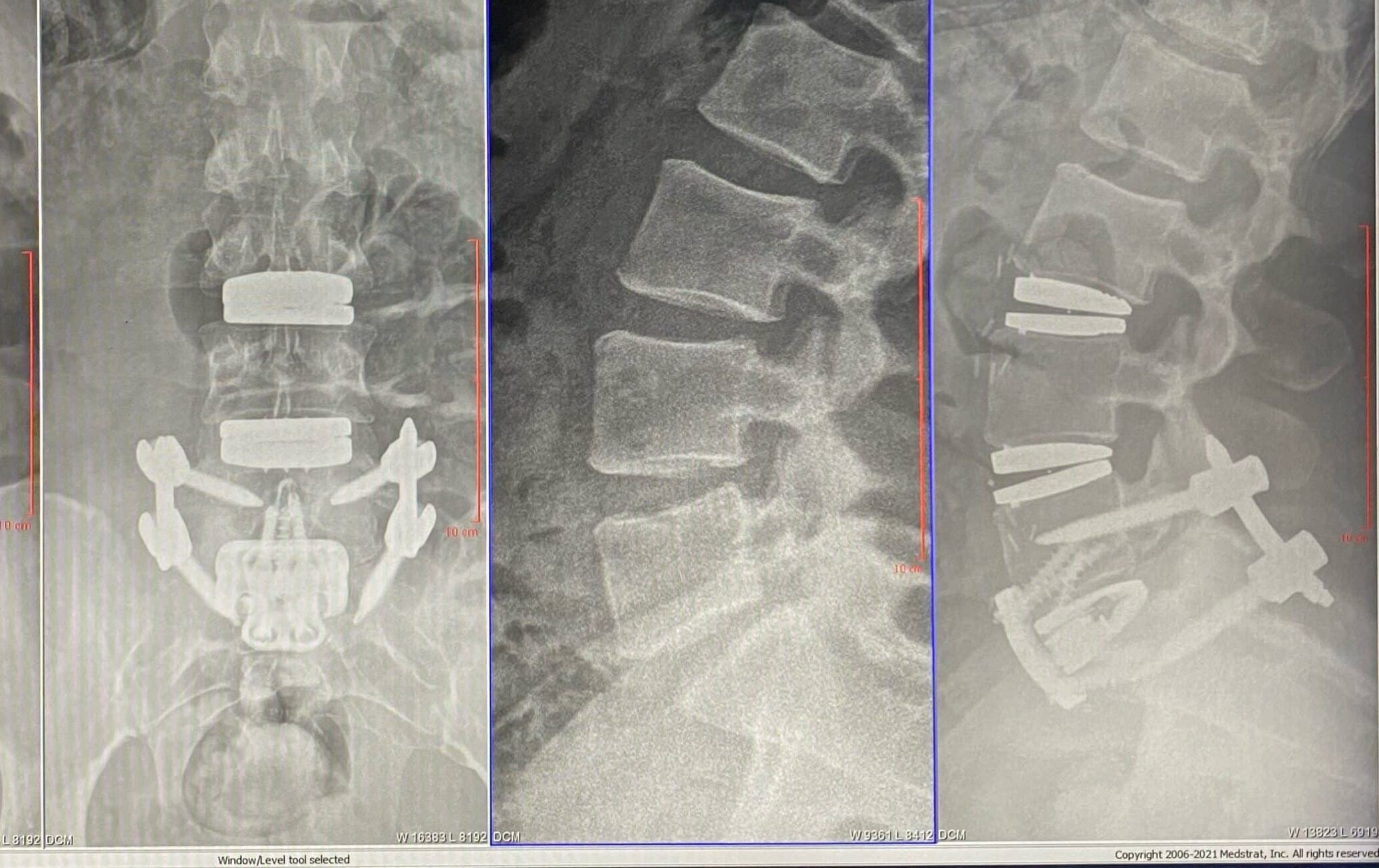
Customizing Surgery to Fit Your Unique Condition
We are able to get our patients back to their pain-free lives faster than ever before. At VSI, we have the ability to customize our patient’s treatments to their individual goals for recovery. Our world-class surgeons are at the forefront of innovative and customized surgery for each unique patient. With our outside-of-the-box thinking, combined with surgical technique and the latest cutting-edge technology, it results in the most effective surgeries with minimized downtime.
Discover the Benefits of Minimally-Invasive Spine Surgery
Minimally invasive spine surgery offers the same post-surgical benefits as traditional spine surgery, but with much less trauma. In recent years, minimally invasive techniques have changed the face of spine surgery and ultimately surgical recovery.
Some common benefits associated with non-invasive spine surgery include:
- More effective surgical outcomes
- Faster recovery time & less post-operative pain
- Shorter hospital stay
- Less anesthesia & radiation exposure during surgery
- Smaller incisions leading to less scarring

Enhanced Surgical Recovery
Enhanced Surgical Recovery (ESR) is a multimodal set of protocols used by your surgical team to help ensure best possible outcomes from your surgery. Important components of ESR occur before, during and after your surgery.
Meet our award-winning surgeons