Working Together
Finding Solutions
Relieving Pain
The Ultimate Choice For Ultimate Spine Solutions®
Explore Our Resources
Empowering Our Patients Through Shared Knowledge

Motion-Preservation Spine Surgery: Disc Replacement and Fusion Alternatives
January 26, 2026
See More
VSI Doctors in Top 7% of Physicians Nationwide in 2026
January 21, 2026
See More
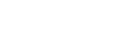
VSI® Performs World’s First Bertolotti Resection Surgery Utilizing Augmented Reality
January 20, 2026
See More
Disc Replacement After Years of Chronic Back Pain: Rachel’s Story
January 7, 2026
See More
Holidays, Hormones, and Headaches: Causes & Relief Tips
December 30, 2025
See More
The Newest Treatment for Spinal Stenosis
December 19, 2025
See More
Lumbar Spinal Stenosis: Do I Need Surgery?
December 19, 2025
See More
Minimally Invasive Options For Spinal Stenosis In The Lower Back
December 19, 2025
See More
Understanding Lumbar Spinal Stenosis: Causes, Symptoms, and Treatment Options
December 19, 2025
See More
Dr. Good on Fox 5: Why Recovery After Spine Surgery Matters Most
December 17, 2025
See More
The Neurologist’s Guide to Coffee Timing: When to Drink Caffeine
December 5, 2025
See More
Understanding Headaches and Migraines: Expert Insights for Finding Real Relief
December 3, 2025
See More
5 Signs You Should Not Ignore Related to Your Back Pain
December 2, 2025
See More
VSI® Performs World’s First Robotic Minimally Invasive Bertolotti’s Resection Surgery
November 25, 2025
See More
Complete Guide to Running for Women: Prevention, Management, and Recovery
November 11, 2025
See MoreJoin The Conversation
#MyVSIVictoryStory
Setting 2026 Health Goals? Listen Up… #supplements #healthgoals #vitamins
How to protect your back while shoveling snow and ice: Tips from a Spine Surgeon
Waking up with hand tingling or neck pain? It could be due to the T-Rex sleep position. #sleeptips
World’s first Bertolotti resection using augmented reality (AR) guidance
3 easy exercises to relieve everyday neck pain. #techneck #neckpainrelief
Before you go all-in in cardio this year, listen up… #corestrength #spinehealth #2026goals
Denied Disc Replacement? How a Second Opinion Changed Her Life
Disc Replacement Surgery for Young Adults #backsurgery #discreplacement #spinesurgery
Why Disc Herniations Come Back After Surgery | Doctor Explains