Segmental Instability
Understanding the Symptoms, Causes & Treatments of Segmental Instability
Reviewed by: Dr. Christopher Good, Dr. Colin Haines, Dr. Ehsan Jazini
What is Segmental Instability?
To truly understand what segmental instability is in the spine, it’s important first to grasp spinal anatomy. The spine consists of bones, discs, soft tissues, and nerves. There are 7 cervical bones, 12 thoracic bones, and 5 lumbar vertebrae, which are circular bones stacked on top of each other, allowing smooth spinal movement.
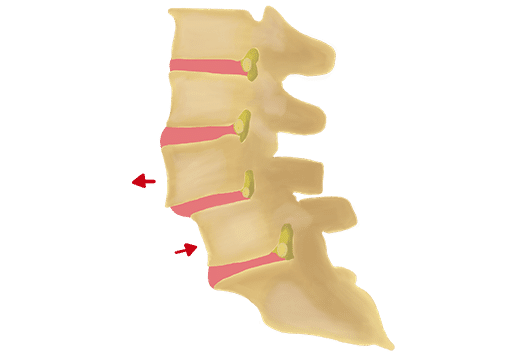
Each level of your spine functions as a three-joint complex: two facet joints and an intervertebral disc. These three components work together like a tripod to create stability, supporting the weight above each level while facilitating motion. Segmental instability refers to hypermobility or a greater-than-normal range of motion between two vertebral segments. This condition often develops when a particular disc or facet joint degenerates to the point that it can no longer support the weight of the body through that segment of the spine.
Spinal hypermobility can result in a hypermobile spine, leading to symptoms that range from mild discomfort to severe pain, particularly in the lumbar region. These issues are often aggravated during forward and backward bending, contributing to hypermobility in the lower back. Common causes include spondylolysis and degeneration of the intervertebral discs or facet joints. Additionally, spondylolisthesis occurs when one vertebral body slips forward over another, which can lead to segmental instability.

What Are Common Symptoms of Spine Instability?
Symptoms of spinal instability vary depending on the severity and location. They can include pain, discomfort, stiffness, or muscle spasms in the lower back. Radiculopathy symptoms may also appear, such as numbness, tingling, pain, or weakness in the legs. If the instability is severe and exerts significant pressure on the spinal nerves, it can lead to cauda equina syndrome. Symptoms of this condition may include loss of bowel or bladder control, urinary urgency, saddle anesthesia (numbness around the groin), and difficulty with balance or walking. Cauda equina syndrome is a spinal emergency, and if you experience these symptoms, seek immediate evaluation.
When to Seek Treatment for Spinal Instability?
If you are experiencing symptoms of segmental instability and suspect a spinal condition, it is essential to consult a board certified spine doctor. Early treatment can significantly enhance your overall well-being and expand your range of treatment options, which may diminish if symptoms persist. Addressing the underlying cause of spinal instability with a specialist as soon as symptoms arise is vital for a successful and efficient recovery.
While many individuals may encounter occasional back pain or neck discomfort and attribute it to minor soreness, persistent pain lasting more than 10 days warrants serious attention. Prolonged discomfort should be evaluated by a spine surgeon to ascertain the root cause and determine the most appropriate treatment. Additionally, be vigilant for other concerning signs related to spinal hypermobility or thoracic instability, such as pain accompanied by fever, loss of bladder control, or weakness, tingling, or numbness in the extremities.
These guidelines reflect our extensive expertise in spine care accumulated over the past three decades, acknowledging that each patient’s presentation may be unique.


What Are Common Causes of Segmental Instability?
There are many other causes of segmental instability of the spine. Spine Hypermobility refers to an abnormal amount of motion or hypermobility across two vertebral body sections. This condition can manifest as one vertebral body shifting forward, backward, or sideways, leading to abnormal spinal alignment. One common form of spine hypermobility is spondylolisthesis, characterized by the forward slippage of one vertebra in relation to the vertebra below. This condition often occurs secondary to spondylolysis, which is a fracture of the pars interarticularis (isthmic spondylolysis).
Thoracic instability is another form of spinal hypermobility that can affect the thoracic spine. There are several causes of segmental instability in the spine, including degeneration of the intervertebral disc or facet joints. The disc and facet joints are crucial components of each motion segment. Another risk factor for spinal hypermobility is a weakened or deconditioned core, which includes the superficial and deep muscles of the abdomen and back. When these muscles, which support the spine, are weakened, the spine is at increased risk for instability. Although rare, instability can also occur in the cervical or thoracic spine following severe trauma, such as a car accident.
Diagnosing thoracic instability often involves performing a thoracic spine instability test and conducting thorough evaluations. Identifying and addressing thoracic spine instability and related spinal hypermobility are crucial for developing an effective treatment and management plan.
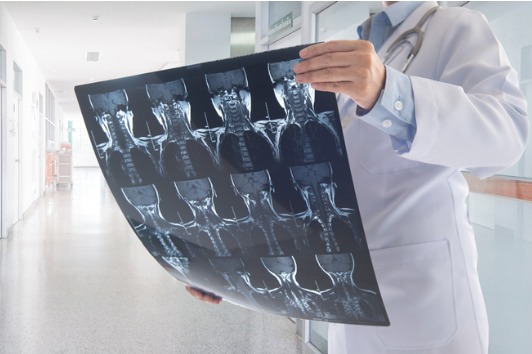
How is Segmental Instability Diagnosed?
Although when evaluating patients we obtain a detailed medical history and perform a comprehensive examination which increases our suspicion for segmental instability it is not diagnosed without imaging. Typical x-rays include weight bearing AP, lateral, flexion and extension views. Sometimes instability is obvious while other times it is not, which is why flexion and extension x-rays are vital. By having a patient bend forward and backwards we are assessing for spinal instability in motion.

What Are Common Treatments for Segmental Instability?
Initial treatment for segmental instability consists of non-surgical treatment modalities including spine-specialized physical therapy, anti-inflammatory medications, core strengthening, low impact exercise, manual massage, and trigger point dry needling. This would help with managing hypermobility back pain.
Surgical intervention may be recommended if you fail non-surgical treatments, develop progressive neurologic deficit, have severe spinal instability, or intractable pain. The goal of surgery is to stabilize the unstable spinal segment which is best achieved through a fusion procedure. The fusion would weld two bones together to prevent further motion or slippage and improve overall alignment and disc height.
Frequently Asked Questions about Segmental Instability
Unclear on hypermobility spine symptoms?
Schedule a consultation with VSI for a detailed evaluation and accurate diagnosis by speaking with our spine doctors. We recommend in-person visits for the best care.