ADR vs. Spinal Fusion: Which Surgery Is Better?
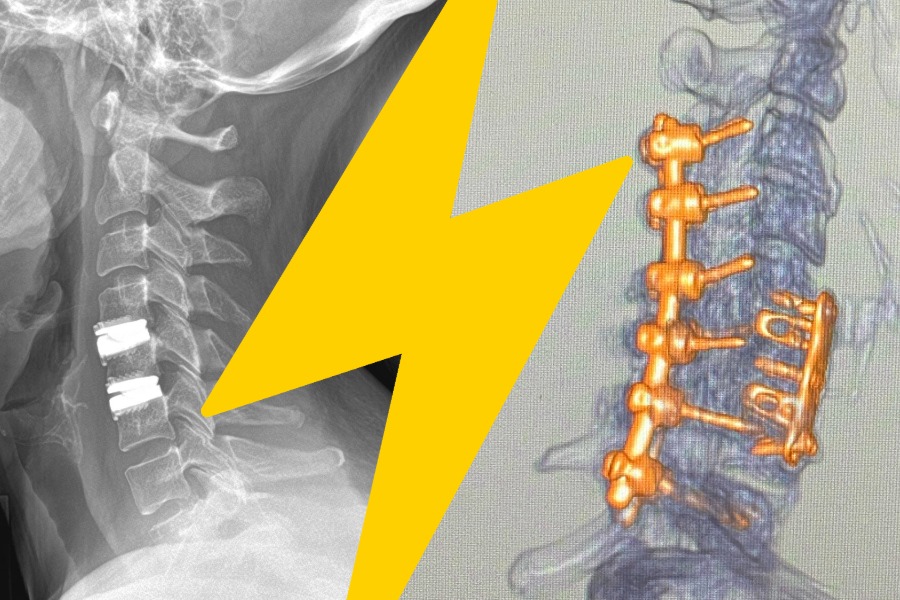
Both ADR (artificial disc replacement) and spinal fusion effectively relieve pain. ADR replaces a damaged disc with an artificial one to preserve motion, while spinal fusion permanently joins vertebrae to stabilize the spine but limits movement.
Quick Answer: Key Differences at a Glance
Both artificial disc replacement (ADR) and spinal fusion are proven surgical solutions for spine pain, but they differ in approach. ADR replaces a damaged disc with an artificial one to preserve natural motion, whereas spinal fusion permanently joins two vertebrae to stabilize the spine, eliminating motion at that segment. In other words, ADR relieves pain while maintaining flexibility in the spine, and fusion relieves pain by stopping movement at the problem level (which can protect unstable or severely degenerated areas). Each has its place — ADR often allows quicker recovery and less stress on adjacent discs, and fusion provides needed stability in certain conditions. Below is a section-by-section breakdown of how each procedure works, their pros and cons, candidate criteria, and how VSI helps patients choose the optimal option.
- Key Difference Summary: ADR preserves motion, Fusion eliminates motion. ADR replaces the damaged disc with an artificial disc that mimics natural movement, preserving motion, while spinal fusion ‘welds’ vertebrae together to stop motion at that level. This means ADR patients keep more neck/back flexibility, whereas fusion patients lose some motion at the fused segment.
- Clinical Outcomes: Both effective, ADR often with equal or better outcomes: A 2019 meta-analysis of randomized trials, published by National Library of Medicine (NIH), found that compared to fusion, total disc replacement had significantly better outcomes in pain and function scores (ODI, VAS, SF-36), with higher patient satisfaction and lower reoperation rates at 5-year follow-ups.
What Is Artificial Disc Replacement (ADR)?
In this VSI Q&A, Dr. Haines explains that artificial disc replacement involves removing the diseased disc and inserting an artificial disc implant that closely imitates a natural disc’s structure and movement. The artificial disc functions as a cushion between the vertebrae, preserving the spine’s normal range of motion (bending and rotating) while eliminating the source of pain (the damaged disc).
ADR is a minimally invasive spine surgery where the surgeon removes the degenerated disc and replaces it with an artificial disc, which serves as a shock absorber and maintains natural motion of the spine.
Conditions ADR Commonly Treats
ADR is most commonly used to treat degenerative disc disease, herniated discs, certain cases of spinal stenosis or radiculopathy, and issues at one level of the spine. Typical candidates have disc problems causing nerve compression (e.g. arm pain from a cervical herniated disc, or lower back and leg pain from a lumbar disc) that have not improved with conservative care. ADR can also be an option for patients with a previously failed fusion at an adjacent level or multi-level disc disease, in order to avoid further fusions.
The Goal: Pain Relief Without Sacrificing Motion
Preserving motion is the primary goal disc replacement. By swapping out the bad disc for a mobile implant, ADR relieves pain while maintaining normal movement, which in turn reduces stress on adjacent levels compared to fusion. This is crucial for long-term spine health: fusion’s loss of motion can increase wear on discs above and below, whereas ADR’s motion preservation aims to prevent that adjacent segment degeneration. In short, ADR offers pain relief and allows patients to stay active with a more natural-feeling spine after surgery.
What Is Spinal Fusion?
How Fusion Works
Spinal fusion is a procedure that “eliminates the motion between vertebrae by ‘welding’ the bones together,” using bone graft and often screws and plates. Essentially, the surgeon removes the damaged disc (and sometimes also relieves nerve pressure by removing bone spurs or doing a laminectomy) and then inserts a bone graft or spacer. Metal screws and rods are typically placed to hold the vertebrae in position while the bone graft heals, eventually fusing the vertebrae into one solid bone unit. This permanent fusion stabilizes that segment of the spine and prevents any painful movement at the affected level.
Conditions Often Treated With Fusion
Spinal fusion is often recommended for conditions where stability is a concern or multiple levels are affected. For example, spinal instability (from spondylolisthesis or trauma), degenerative disc disease affecting multiple levels, spinal deformities like scoliosis or kyphosis, severe spondylolisthesis, fractures, and spine tumors or infections are often treated with fusion. In these cases, fusing the vertebrae can restore proper alignment and stabilize the spine.
Why Fusion Is Still Necessary in Some Cases
“Stability vs. Motion”
We emphasize a balanced, patient-first approach: When we can preserve motion, we do. When stability is required, then fusion is still a good option. In other words, if a spine segment is too unstable (e.g. due to a fracture, severe slippage, or after removal of bone in a decompression) or if there’s extensive degenerative change that an artificial disc can’t overcome, fusion is recommended to prevent neurological damage and pain. Fusion provides a reliable solution in cases where ADR isn’t feasible – such as severe osteoporosis (weak bone that can’t support an implant), advanced facet joint disease, or when correcting deformities.
Hybrid Combination Surgery Approach
At times, combining both techniques (hybrid surgery) by fusing the most unstable level and replacing adjacent discs can provide the best of both worlds and produce excellent results compared to fusion only. VSI patients have experienced significant success through the combination of these treatment options. Fusion remains necessary and appropriate for the worst levels of instability or deformity, even as motion-preserving options expand.
ADR vs. Spinal Fusion: Side-by-Side Comparison
Motion & Function
ADR’s biggest advantage is that it preserves the normal motion of the spine at the operated level. Patients who undergo disc replacement in the neck, for example, lose virtually 0° of motion at that level because the artificial disc moves with the spine. In contrast, fusion by definition stops movement – roughly 10 degrees of motion is lost per level fused in the cervical spine (and similarly in the lumbar spine). This loss of motion in fusion is not usually functionally disabling (especially if one level is fused, patients still have overall good range of motion), but ADR patients often report a more “natural” feel in their spine movement after recovery. As VSI surgeon Dr. Haines notes, maintaining motion with ADR means forces during movement are evenly distributed across the spine, rather than concentrated above/below a fusion. This may help reduce wear on adjacent segments.
Adjacent Segment Stress
With fusion, the segments next to the fusion take on extra strain, which can lead to “adjacent segment disease” over time (accelerated degeneration next to a fusion). Clinical studies have observed that after a cervical fusion, about 25% of patients show adjacent segment deterioration within 10 years, as stated in the Spine-Care Journal. ADR was designed to mitigate this issue by preserving motion and lessening the likelihood of adjacent discs breaking down. In terms of motion and overall spinal function, ADR keeps the spine moving naturally whereas fusion sacrifices motion for the sake of stability.
Pain Relief & Success Rates
Effectiveness: Both ADR and fusion are effective at relieving nerve compression and mechanical pain from a diseased disc. Large studies show no significant difference in basic pain relief outcomes (both procedures markedly improve patients’ pain scores and disability indexes) in appropriately selected patients. However, some recent evidence suggests ADR patients may experience equal or better functional improvement. This implies that on average, ADR can match fusion for pain relief, and often leads to superior patient-reported outcomes, likely because they retain mobility and recover faster.
Success Rates: VSI surgeons have noted high success in their ADR patients. Dr. Haines states “success rate is over 95 percent” for cervical disc replacement in appropriately chosen candidates. Spinal fusion success rates are also high (commonly in the 90% range for single-level fusions relieving the intended pain). The biggest takeaway is that both surgeries have high success rates for improving quality of life. ADR may confer some advantages in patient satisfaction and functional scores, as preserving motion often leads to a faster recovery to normal life. Meanwhile, fusion remains a tried-and-true solution with decades of patient data behind it.
Recovery Time & Return to Activity
ADR Recovery
Because no bone needs to fuse in ADR, the initial healing is generally quicker. Patients undergoing cervical disc replacement often go home the same day or after one night, resume light daily activities within a few days, and usually return to desk work or moderate activity within a few weeks. here is typically less post-op bracing required (some don’t need a collar for cervical ADR), and because motion is preserved, patients experience less stiffness.
Fusion Recovery
Fusion involves a bone-healing process that takes time (bone graft integration can take 3-6 months or more). As a result, fusion patients have more activity restrictions in the first few months. A typical hospital stay is 1–3 days (depending on the extent of surgery). Initial recovery includes a few weeks of limited activity: patients must avoid heavy lifting, bending, or twisting while the fusion is setting up. Full return to strenuous activity or sports can take 3–6 months (or longer for multi-level fusions). Many fusion patients wear a brace for several weeks. Overall, return to work is slower: desk jobs might be 4-6 weeks post-op if one-level, and manual labor jobs may require 3+ months before clearance. VSI’s fusion prep guide emphasizes realistic expectations: healing is gradual, with physical therapy often starting only after the initial 6–12 weeks of bony healing. Dr. Good has pointed out that with modern techniques and comprehensive recovery at VSI, even fusion patients can recover faster than in decades past.
Long-Term Risks & Reoperations
Fusion Long-Term Risks: The primary long-term concern after fusion is Adjacent Segment Disease (ASD) – the accelerated degeneration of discs and joints next to the fusion, due to altered biomechanics. Studies from NIH indicate that after cervical fusion, about 2–3% per year of patients develop new issues at adjacent levels, totaling ~25% at 10 years as mentioned above. (Use VSI failed surgery page)
ADR Long Term Risks: On the whole, reoperation rates for ADR and fusion have been found to be comparable or slightly in ADR’s favor at 5-10 years.
Who Is a Good Candidate for ADR vs. Fusion?
Candidate Profile for ADR
Ideal ADR candidates at VSI are patients with single-level or two-level disc disease without significant instability or facet joint arthritis. Dr. Haines notes that if neck pain is coming primarily from a bad disc (not from arthritic facet joints), and the patient has a well-aligned spine, cervical disc replacement can be an excellent option. Similarly, for the low back, those with a herniated or degenerated disc at one level (with preserved facet joints) are evaluated for ADR. Other criteria include good bone quality (no severe osteoporosis) and generally healthy lifestyle (non-smoker or willing to quit, to aid healing). Lack of major deformity is important – if the spine has normal alignment, ADR is feasible, but if there’s a big collapse or slip, fusion might be needed.
Candidate Profile for Fusion
Patients with more complex or degenerated disc issues often require a fusion. These could include:
- Multi-level disc disease: If three or more levels are degenerated and causing symptoms, ADR is usually not approved for so many levels – fusion (or a hybrid of multiple fusions/ADRs) may be indicated.
- Severe facet joint arthritis: ADR doesn’t address facet pain and preserves motion (which would continue to aggravate arthritic facets), so patients with facet-mediated back or neck pain do better with fusion, which stops the motion at those painful joints
- Spinal instability or spondylolisthesis: If a vertebra is slipping (e.g., due to a pars fracture or severe disc collapse), fusion is often required to stabilize it.
- Spinal deformity: Cases of scoliosis or kyphosis often necessitate fusion to correct alignment. ADR cannot correct significant curvature or tilt of the spine, whereas fusion instrumentation can realign the spine.
- Prior surgery: Patients who have had a laminectomy that removed too much stabilizing bone, or those with a previous fusion adjacent to the level in question, might need a fusion. Also, if someone already had an ADR at a level that failed, the revision is typically a fusion.
- Poor bone quality or other contraindications: As noted, severe osteoporosis means an implant might not seat well – fusion with bone cement or other techniques may be safer. Similarly, certain anatomies (like very small vertebrae) might not accommodate currently available artificial discs.
Age, Activity Level & Lifestyle Considerations
Rather than drawing hard lines based on age or sports goals, our framing is practical: the goal of both ADR and fusion is to get patients back to their normal lives without ongoing limitation. Either outcome can be achievable, but the deciding factor is what the patient’s body and spine anatomy are asking for, particularly whether motion can be safely preserved or whether the segment needs stabilization.
Risks, Complications & How We Reduce Them
The risks and complications associated with ADR and fusion surgery are similar to the risks associated with any spine surgery.
ADR-Specific Risks
A key ADR-related concern is the possibility of future pain driven by instability, especially if the spine segment below isn’t an ideal motion-preservation candidate. We do not see the artificial discs themselves “breaking down,” and when problems occur, they are more often related to the biomechanics of the segment (not the device).
Fusion-Specific Risks
One of the major longer-term considerations with fusion is the potential for breakdown at other levels over time, as the spine redistributes motion and stress to segments above and below the fused area.
How VSI Minimizes Risk
VSI has several strategies and technologies to reduce surgical risks and complications:
- Advanced Technology (Robotics, Navigation, AR): VSI is a national leader in adopting cutting-edge surgical technology. Dr. Christopher and his team have pioneered the use of robotics and augmented reality (AR) guidance in spine surgery, which increases accuracy and safety. In a press release, VSI noted that AR allows for “precise navigation, minimizes tissue dissection, and increases accuracy, potentially leading to fewer complications, reduced blood loss, and faster recovery.” Robotics and computer navigation similarly ensure optimal implant positioning in ADR or fusion, which lowers the risk of things like implant migration.
- Surgeon Expertise and Planning: All cases at VSI are evaluated by experienced spine surgeons, and for complex scenarios, they utilize a team approach (spine surgeons, neurologists, rehab specialists). This review process helps in choosing the right treatment for each patient, thereby avoiding unnecessary procedures and matching patients to the procedure with the least risk for them.
- Patient Selection and Customization: VSI’s philosophy “motion-preservation-first” means they carefully screen who is suitable for ADR vs fusion. By rigorously evaluating factors like facet joint status, bone density, alignment (via imaging and even motion X-rays), they only perform ADR on ideal candidates, which is why their complication rates for ADR are very low. If a patient doesn’t meet criteria, they won’t push an ADR just for the sake of it – they’ll recommend fusion or hybrid if safer. This tailored approach (choosing the right operation for the right patient) inherently minimizes risks like ADR failures or fusion non-unions.
- Enhanced Recovery Protocols (Recovery Revolution™): VSI has implemented a comprehensive recovery movement to speed healing and prevent complications. This includes prehab (so patients are in the best shape going into surgery) and integration of physical therapy, nutrition, and even recovery therapies soon after surgery. All of these measures collectively reduce complication rates and improve outcomes.
What to Expect Before, During & After Each Surgery
Pre-Op Evaluation
VSI emphasizes a thorough consultation process for disc replacement candidacy, including detailed history, hands-on exam, and review of imaging (X-rays and MRI), with ample appointment time to cover diagnosis and create a custom plan.
Day of Surgery: ADR vs. Fusion
Recovery Timeline
Fusion: VSI provides a structured recovery timeline (initial 4–6 weeks; significant healing 3–4 months; full recovery 6–12 months) and activity restrictions (avoid bending/twisting; avoid lifting >8–10 pounds; avoid strenuous/high-impact activity).
Disc replacement: VSI states recovery can be faster compared to fusion when paired with ERAS protocols and spine-specific rehab.
How VSI Helps Patients Choose the Right Option
Keeping You in Motion
VSI’s solutions content repeatedly reinforces this core question: when the spine can be preserved safely, we keep it active and reserve fusion for when stability is required.
Cross Review
VSI describes coordinated care across a “comprehensive suite of specialties,” emphasizing streamlined collaboration and communication so patients aren’t forced to navigate multiple opinions and practices on their own. VSI also highlights collaboration between an in-house neurologist and other clinicians as part of tailored diagnosis and treatment planning.
When We Still Recommend Fusion
Our message is straightforward: fusion remains the right solution when stabilization is required.
When to Talk With a VSI Spine Specialist
If you’re weighing ADR vs. fusion, the most productive next step is a specialist review focused on: (1) your imaging, (2) segment stability, (3) facet joint health, and (4) your motion goals. Above all else, we want to ensure the right treatment for your individual needs and ensure you are a partner in the decisions of your spine health. This is the philosophy that has shaped our relationship with our patients and getting them back to the lives they deserve.
Topics covered
About the Author
Featured Resources
Insights to Achieve a Pain-Free Life